With the approaching conclusion of the Public Health Emergency (PHE), many states are seeking a partner to address challenges impacting Medicaid programs with a significant backlog in eligibility redeterminations.
Public Consulting Group (PCG) can assist Medicaid agencies with the following services:
![]()
Data Services
36 states (and counting) have chosen PCG to manage their access to, and evaluation of, third-party data used to support public assistance eligibility determinations. PCG features fully configurable, out-of-the-box systems which apply state-specific eligibility policy to third-party data results to instantly predict member eligibility across every public assistance program.
![]()
Staff Augmentation
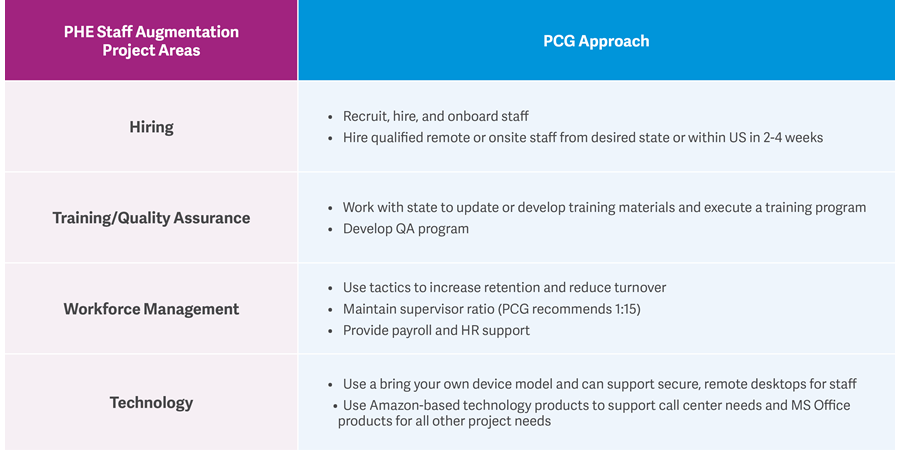
PCG can recruit, train, and manage human capital resources to augment current eligibility staff to assist with redetermination efforts. Our eligibility staff can be virtual or on-site and can support enrollment and eligibility processes, including determining best addresses, sending and processing notices, and call center support for communication and outreach to members.
![]()
Replacement Insurance
PCG can help states identify and manage the members who no longer qualify for Medicaid and work with them to find alternative replacement insurance that meets their needs.
Our Services
Data Services
PCG is a trusted partner in managing a state’s access to third-party data informing more accurate and efficient Medicaid eligibility redeterminations. PCG is data provider neutral, allowing us to provide the best data with proven, automated eligibility verification.
Identify Member Eligibility Across All Public Assistance Programs
With our fully configurable SAAS-based system coupled with proven third-party data sources, PCG can instantly predict eligibility across every public assistance program based on state-specific policies. Currently used by 10 of the largest public assistance programs, PCG reports on and quantifies to level of ineligibility risk each member represents.
Identify Member Locations
PCG has solved the member locating dilemma by adopting the National Change of Address (NCOA) database combined with a leading data provider’s best address, phone (including mobile), and email data service. PCG can manage agency communication to members, allowing real time interaction and further reducing the number of members unnecessarily disenrolled.
Identify Current Ineligibles due to Deceased, Out-of-State, and/or Incarcerated
It is critical to understand the size of your covered population. PCG can help in assessing the size of your Medicaid population and reductions in population to inform unwinding resource planning and redetermination workloads.
Enhance your Ex Parte Renewal Process
PCG maintains a configurable menu of unique data assets that have been proven to support more accurate agency ex parte Medicaid renewals and mid-year SNAP renewals. PCG can improve and enhance the accuracy of the ex parte renewal process and reduce eligibility staffing requirements associated with redetermination and renewal activities.
Automate Renewal Documentation Processing
PCG can automate the process of reviewing, extracting, indexing, tagging, and entering information found on member-submitted renewal correspondence, saving HHS agencies critical time and manpower while improving accuracy. This will allow you to nearly eliminate the eligibility staff time associated with reviewing member submitted renewal documentation, further automating the process and improving access.
Transition Traditional Members to the Exchange Population
For states who have chosen to expand Medicaid, PCG can perform a series of data checks to identify any existing members whose eligibility has changed such that they are no longer eligible for traditional Medicaid but are still eligible for Exchange Medicaid. PCG can assist in finding alternative coverage for members who are no longer eligible for traditional Medicaid.
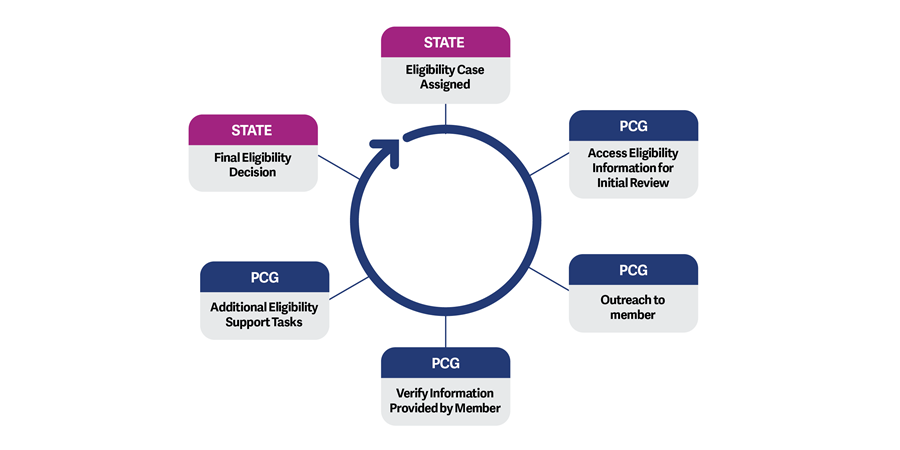
Staff Augmentation
Most Medicaid eligibility programs are dealing with a depleted workforce and a tight labor market at a time when there is a significant increase in case volume due to the continuous enrollment condition for Medicaid and CHIP beneficiaries during the PHE.
PCG can recruit, onboard, train, and manage human capital resources to augment current eligibility staff without obligating the state to retain these positions and related costs beyond the temporary need. PCG has provided staff augmentation services to state HHS agencies for 36 years and can provide onsite and virtual teams to augment local and state eligibility teams. Our eligibility staff can support enrollment and eligibility processes, including notices, data support, and communication and outreach to assist the state with all activities prior to final determination.
PHE Staff Augmentation & the PCG Approach:
Transitioning Previous Medicaid Members to Replacement Insurance
PCG can help states identify and manage the members who no longer qualify for Medicaid and work with them to find alternative replacement insurance that meets their needs.
Our Experience
Staffing Services
Maine OMS Enrollment Broker/Member Services and MaineCare Operations
Handled 9,405 calls per month

New York State Department of Health (NYSDOH) Contact Tracing Initiative
Hired and managed 8,000 staff

NYSDOH Professional Assistance for New York State’s Medicaid Initiatives
Hired and manage 300 staff

MassHealth Eligibility Application Processing and Customer Service Operations Support
Hired and managed 50 staff handling 12,000 calls per month
Michigan Department of Health and Human Services Medicaid Eligibility Quality Control Project
Performed over 800 eligibility review audits
Recently Awarded: Maine Department of Health and Human Services Eligibility and Enrollment Support Services
Will provide 50 staff to assist with eligibility support functions
Recently Awarded: Montana Department of Public Health and Human Services Medicaid Eligibility Staff Augmentation
Will provide 40 staff to assist with eligibility support functions
Data Services
On behalf of a top three public assistance program, PCG processes nearly 1 million daily transactions accessing different combinations of commercial, state, and federal data sources through a single interface, each of which results in the near-instantaneous creation of a single on-screen HTML report featuring consolidated, organized results, data, and “case clues” within the agency’s integrated eligibility system.
To assist in unwinding after the PHE, PCG is connecting another top 10 public assistance program to the most useful data competing commercial vendors offer through a single interface with PCG. PCG’s product can predict eligibility for every configured public assistance program, including their Exchange program, prior to an eligibility technician touching the case.
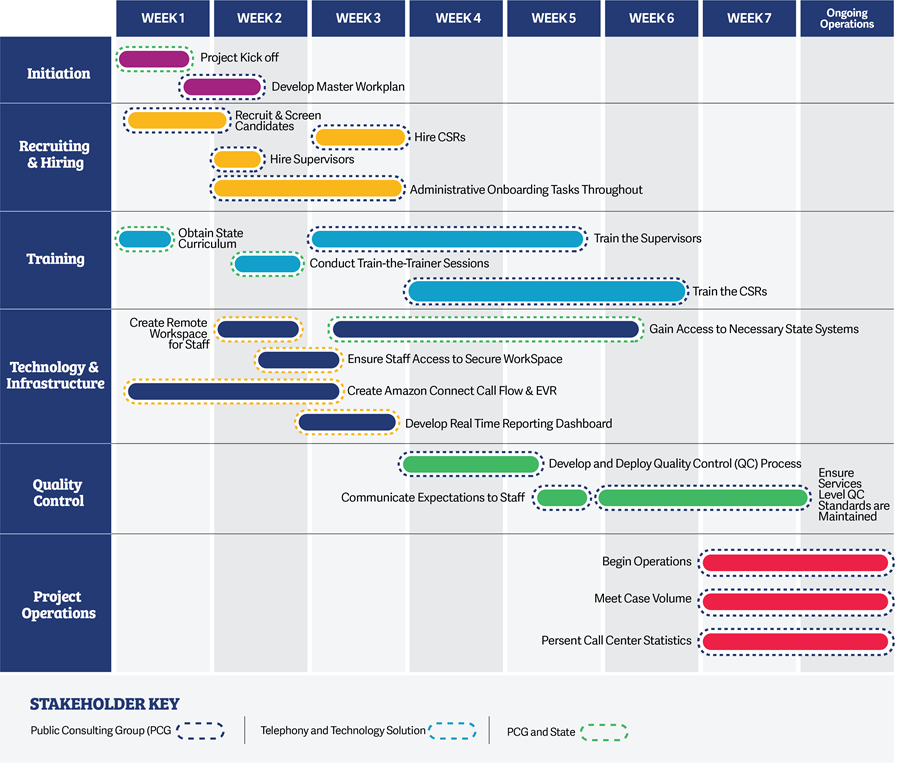
Project Management and Implementation
A key advantage to selecting PCG as a partner is our organized and disciplined approach to project management. Working almost exclusively with state government agencies, we fully understand and appreciate that—on the state side of the equation—obstacles arise, directions change, and resources can be diverted or constrained. This is all the more reason that—on the vendor side of the equation—OFI needs a partner that is organized with a plan that is adjustable on demand, and adept at refining and improving procedures accordingly.
At PCG, we provide senior consulting staff who have extensive experience with Medicaid eligibility work and staff augmentation projects. Our project team will lend expertise and lessons learned from our other engagements to ensure our clients benefit from previous solutions implemented on similar projects. We believe that the combined strengths, skills, and experience of our team sets us apart from our competitors. Staffing Solutions Organization (SSO), a PCG company, includes experienced recruiting professionals, member eligibility and implementation specialists, and project management professionals.
Below is a sample implementation schedule for our PHE Unwinding Staff Augmentation services: