For more than 34 years PCG has been providing management consulting services to public sector clients across the United States, Canada, and Europe. As your TPA, these services are at your fingertips. Tap into our public sector expertise in the areas of:
Payment Transformation
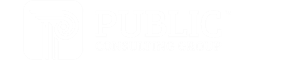
PCG helps our payers and providers advance their reimbursement strategies across the payment maturity scale.
SOURCE: Health Care Payment Learning & Action Network
Let PCG help you create your Payment Transformation Road Map:
- Analyze Data to identify opportunities and establish prioritized Focus Areas
- Perform Episode Design Modeling to tailor a program to meet the needs of CCA and its populations
- Model Payment Scenarios and assess fiscal implications
- Develop a VBP Roadmap to achieve standardization and administrative simplification
- Train Providers
- Operationalize, support, and monitor payment transformation efforts
Rate-setting
Not everyone is ready for sophisticated, risk-based reimbursement methodologies. PCG is an industry leader in establishing and updating cost-based rate setting and cost settlement services, as well. We have:
- Implemented numerous groupers to reform inpatient hospital payments, including AP-DRGs, APR-DRGs, and MS-DRGs
- Experience reforming outpatient hospital reimbursement systems from cost-based methodologies to acuity and resourced-based payment methodologies (APCs and EAPGs)
- Overhauled community-based reimbursement schemes through analysis of population demographics and accurate accounting of non-institutional health care costs
- Optimized crossover claims pricing logic to minimize payer expenditures
- Ensure payments are limited to the Medicaid allowed amount by developing appropriate pricing algorithms
Cost Reporting and Cost Accounting
PCG has a team of Medicare and Medicaid cost reporting experts, with experience completing and auditing cost reports for hospital, nursing facility, ICF/IID, community mental health centers, FQHCs, and substance abuse providers, among others.
PCG can:
- Design cost reporting forms to understand the actual cost of healthcare services
- This includes automating Medicaid cost report requirements through the deployment of proprietary web-based cost reporting software
- Analyzing Medicare and Medicaid cost reports to understand cost drivers
- Analyzing cost reports to assess payment adequacy
Payment Variability Analysis
PCG can help ensure that networks include only the most efficient and effective providers. PCG can assess potential cost savings by evaluating payment variability across the network which can also help achieve network optimization.
PCG can quickly analyze variability among your providers to:
- Identify the median payment by procedure code and provide benchmark comparisons to pinpoint high cost and high-volume providers
- Allow for analysis to quantify potential cost savings by renegotiating payment levels or redirecting care to other providers
- Empower staff to redirect care to other low-cost providers
- Provide price transparency information across the organization
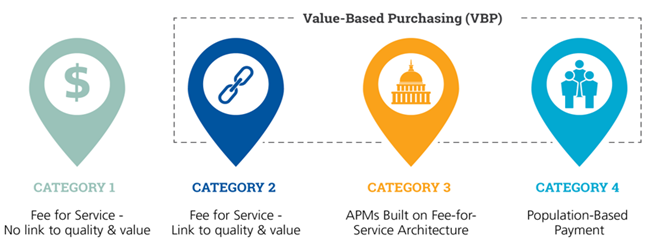
Program Integrity
PCG’s innovative approach to Payment Integrity is specifically designed for the Medicaid HCBS provider population. Rather than large-scale, long-term audits geared toward recoupments, PCG reviews are quick and focused, geared toward accountability and quantifiable future cost avoidance.
Choose from a menu of Program Integrity options that fit your needs.
Provider Enrollment and Support
Process network enrollment applications, manage provider directories, deliver provider support via call centers and web
Provider Screenings and Database Checks
ACA requires that all high- and moderate-risk providers undergo fingerprint and background checks
Due Process Oversight and Monitoring
PCG can manage and deliver all appeals for reduction or denials in level of care, eligibility, or services
Provider Onsite Screening Visits
ACA requires Medicaid conduct onsite visits for all high- and moderate-risk providers. With more than 6,000 onsite visits completed, PCG has screened out more than 1,000 unqualified providers
Routine Reviews
Brief, high-touch, frequent regular reviews of providers to ensure compliance with policy and code. Ensure proper staffing, plans of care, level of service, and detect fraud, waste, or abuse. Focus on correction, education, and cost avoidance.
Investigations
Respond to complaints and reported incidents to ensure compliance and health and safety of beneficiaries. Focus may be on individual and/or provider.
Initiated within 48 hours, average 15 hours to complete, and are closed within 45-60 days.
Prepayment Reviews
Flag high-risk claims and providers for pre-payment review. Review supporting documentation for claims after submission, but prior to payment.
Post Payment Audits
Conduct full-scale audits using data analytics, sampling and extrapolation to recoup large over-payments where payback is likely, and the provider is prepared and qualified to continue to deliver services.
Hundreds of millions of savings and cost avoidance found for our clients
Public Program Management
PCG can help evaluate the efficiency and effectiveness of programs and targeted interventions.
- PCG has years of experience assessing the efficiency and effectiveness of State Medicaid programs.
- PCG has helped design and/or implement delivery system reform incentive payment programs.
- Service assessments have identified gaps in service need and to determine if the goals of the programs are being met.
- Pre- and post-intervention utilization and payment analysis yields insights into the effectiveness of interventions and programs.
- Policy, utilization, and financial analyses contributes toward program redesigns and organizational strategic planning efforts.