Data Intermediary Solution - Hospital All Payer Claims Reporting System
PCG has developed proprietary web-based technology to support government agencies in the collection of inpatient and outpatient hospital claims data to inform public health officials about important healthcare trends. With PCG’s data intermediary solution (DIS), our state clients have a highly customizable web-based application that employs modern data infrastructure and security technologies, intuitive and efficient front-end user interface and user experience (UI/UX), automated workflow features, comprehensive clinical claim edits, and flexible reporting to collect and process all-payer inpatient and outpatient hospital and ambulatory surgical center claims data. PCG’s web-based technology enables state agencies to: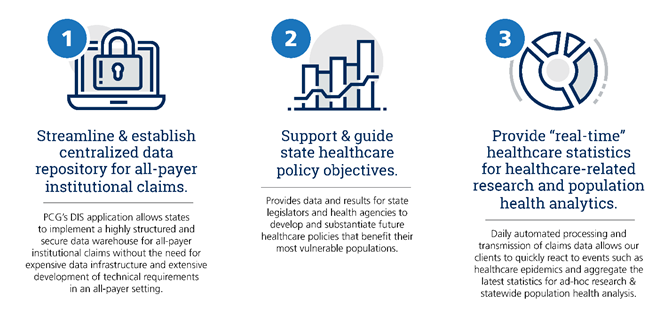
While highly customizable, PCG’s DIS application also contains a variety of standard features “out-of-the-box” that can immediately provide significant value:
- Secure user access with HIPAA-compliant accounts and data safety considerations
- Role-based application dashboard with file and claim related statistics widgets
- Flexible user management functionalities with distinct and combined pre-determined user roles
- Provider information and contact management
- Web-based file upload for provider HIPAA-compliant standard and customized 837 (I, P, R) transaction processing claim files
- File submission documentation and statistics analytics
- Comprehensive claim clinical edits (e.g. MCE, OCE, NCCI, MUE)
- UI-based claim error revision and resubmission
- Standardized geocoding of submitted claims
- Inpatient and outpatient claim grouping capabilities (i.e. 3M APR-DRG, MS-DRG, 3M EAPG, APC)
- Easy to use claim search and review
- Canned file submission and claims statistics reports
- Accepted claims data extract automation for submitting providers
PCG’s DIS application, along with our supporting implementation consulting services, differentiates itself through its modern, intuitive UI and application infrastructure, extensive collection of standard features, comprehensive implementation support and training, and streamlined vertical integration of claims collection, processing, editing, and reporting capabilities.
National Impact

Currently, more than 5 million all-payer inpatient and outpatient institutional claims are processed annually from over 120 hospital providers to support healthcare policies that will benefit more than 9 million people across the nation. Contact us today to learn more about your hospital claims system needs!
